Why Our Ever-Evolving Genes Sometimes Make Us Sick

We all develop mutations in our genes as we age. Like typos in our genetic code, these mutations begin to accumulate almost from the moment of conception. Many mutations have no impact at all, but some increase our risk of disease. The trouble is that it is hard to tell which mutations matter and which do not. That’s where geneticist Maria Pokrovskii comes in.
Pokrovskii, who is in her second year with the Simons Society of Fellows, is an expert on the interaction of genetics, immunity and disease risk. She earned a bachelor’s degree in molecular and cell biology from the University of California, Berkeley in 2005. After cutting her teeth at biotech firms in the San Francisco Bay Area, Pokrovskii returned to academia, earning a doctorate in immunology at New York University in 2018 under the mentorship of Dan Littman. At NYU she and her colleague Mo Xu discovered a surprising example of the gene-immunity connection in the gut. In work published in the journal Nature, the team identified a group of immunity-boosting genes that, when impaired, leads to dangerous conditions such as Crohn’s disease, a chronic inflammatory bowel disease that affects the lining of the digestive tract.
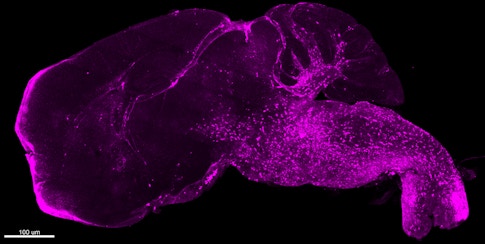
Now a postdoctoral fellow in Frederic Geissmann’s lab at the Memorial Sloan Kettering Cancer Center, Pokrovskii has shifted her focus from the gut to the brain. She studies how genetic mutations in the brain’s innate immune system might result in neurodegenerative diseases such as Alzheimer’s disease. Pokrovskii focuses on mutations that we do not get from our parents, known as somatic mutations.
Pokrovskii and I spoke recently about the value of serendipity in scientific discovery, the interplay between genetics and environmental factors, and what she is learning about the connection between mutations and brain disease. Our conversation has been edited for clarity.
Why is it challenging to discern the connection between our genetic makeup and disease risk?
It is very hard to isolate the role of genetics in causing disease. Some diseases could be caused by somatic mutations, which arise soon after conception. Other diseases might be caused by inherited mutations from our parents or by environmental factors, such as exposure to disease-causing toxic substances like asbestos, as well as the impact of life stresses and diet on someone’s disease risk.
Identifying a particular somatic mutation, and then proving it has causal link to disease, is challenging because most somatic mutations have no bad effects at all. It’s a bit like looking for a needle in a haystack.
You can think of our genes as the body’s blueprint. Our genetic code influences much about what we look like, like our eye color and height. In broad terms, the same gene plays the same role for most people. But that’s a bit too simplistic. How a gene works in any given person depends on what version they received from their parents, as well as any somatic mutations that arise along the way. Compounding this complexity is the fact that somatic mutations only affect the cells in which that mutation occurs, as opposed to all cells throughout the body.
One example in which somatic mutations can cause havoc in tissues is in many forms of cancer. But many environmental factors, such as exposure to toxins in food or water, also influence cancer risk. For example, research has shown that the presence of arsenic in drinking water increases one’s risk of developing bladder or lung cancer.
In short, it’s relatively rare for an inherited mutation alone to be a driver of disease. I am focused on the role of somatic mutations because I think they may explain some of these diseases for which we don’t know the cause.
What discoveries have you made so far along these lines?
While completing my doctorate at NYU I experienced a wonderful instance of scientific serendipity. In studying genes that control immune functions in our gut, I had found one gene (known as c-MAF) linked to anti-inflammatory immune cells called Treg cells. Anti-inflammatory cells are so called because they manage inflammation, which helps prevent things like joint pain. But I wasn’t sure exactly how it all fit together — specifically, which inflammatory conditions c-MAF Treg cells helped control. By coincidence, my lab colleague Mo Xu was exploring why a species of gut bacteria that is harmless in most people and mice occasionally causes conditions like Crohn’s or ulcerative colitis, a related autoimmune disease. And as it turned out, this is where the answers to my own research question resided: just a few feet away at Mo’s lab bench.
We found that healthy mice in Mo’s experiments used c-MAF genes to produce Treg cells to keep themselves healthy; when we disrupted the development of those cells, that’s when trouble occurred. In 2018, we published this discovery in Nature.
Serendipitous indeed! What drew you to the Geissmann lab for your postdoc at Sloan Kettering?
When I was still at NYU some members of the Geissmann lab published a paper showing that a somatic gene mutation alters the brain’s immune cells, which are known as microglia. This then causes other brain cells, namely neurons, to die.
Whoa! Here was a new way to think about neurodegenerative diseases such as Alzheimer’s. It’s well established that these diseases occur when neurons get damaged or die, but the role of somatic mutations and of microglia is much less understood. After reading that paper, I knew I wanted to study the role of immunity in neurodegenerative diseases, in hopes that this approach can eventually lead to much-needed cures. Alzheimer’s makes a particularly strong candidate for this approach, because almost every treatment that seemed promising has failed in clinical trials.
Why have Alzheimer’s treatments been so hard to develop?
Alzheimer’s is almost unmatched in its complexity. For a long time, researchers thought that addressing the most obvious manifestations of Alzheimer’s — the buildup of unusual plaques and tangles in the brain that seemed to be eating away at neurons — would solve the problem. Just develop a drug that stops the tangles and plaques, the thinking went. But more recently, experts found that different people manifest Alzheimer’s differently.
There are a few cases of inherited early-onset Alzheimer’s. But most instances of Alzheimer’s are late-onset, and we don’t know their cause. Many researchers think that a combination of inherited traits and environmental factors lead to late-onset cases. By contrast, our lab has proposed that somatic mutations in microglia could lead to Alzheimer’s in some people. This immunity-centric hypothesis is somewhat controversial, so we are testing to see if it holds up.
How are you testing this hypothesis?
We think that microglia from the brains of Alzheimer’s patients may indeed contain somatic mutations that we don’t see in the brains of healthy individuals.
To find out more, I’ve introduced these somatic gene mutations into lab mice. I am now monitoring them as they age to see if they exhibit signs of Alzheimer’s. If the mice develop neurodegeneration or worse memories, we can confidently say that this gene mutation was the cause. I’m in the wait-and-see stage right now.
Well, I guess that patience is a virtue. What do you plan to do after your postdoc concludes?
Postdoc appointments in immunology and biology can take an average of five years. I’m about halfway through mine, but I’m not sure how long my experiments will take! In a few years I hope to move on to an independent academic position where I can develop ways to run these kinds of experiments more quickly. For example, I’d love to build tools that can distinguish which mutations will become harmful — and how they will cause harm — so we can avoid having to wait for mice to age before we draw any conclusions.